Are toddlers meeting the New Canadian 24-Hour Movement Guidelines for the Early Years?
December 12, 2017
Benefits to heart health of reducing workplace sitting
February 16, 2018Today’s post comes from Dr Paddy Dempsey. You can find more about Dr Dempsey’s work at the bottom of this post. To request copies of the papers described in this article, visit his profile on ResearchGate.
Globally, over half a billion people are projected to have type 2 diabetes (T2D) by 2035, around 10% of the population. In Australia alone, around 280 new people are diagnosed with T2D every day – costing the healthcare system >$14 billion/year. It is a major cause of premature mortality and morbidity due to cardiovascular, renal, ophthalmic and neurological disease. Accordingly, safe, effective and sustainable approaches are urgently needed to curtail, but also manage, the growing T2D epidemic.
Physical activity is key for T2D prevention and management
While regular exercise is an effective tool in preventing and managing T2D – particularly for glucose metabolism, blood pressure and insulin sensitivity – meeting prescribed aerobic and resistance (strengthening) exercise guidelines can be challenging, and most remain physically inactive.
Moreover, in developed countries and in the rapidly urbanizing populations of developing countries, sedentary behaviours (too much sitting as distinct from too little exercise) have become the default behavioural option – inextricably embedded in work, school, transport, and leisure.
Finding beneficial and practical alternative strategies – observational and emerging experimental research insights
The good news is that epidemiological, and more recently, experimental research evidence, indicates that simply reducing and ‘breaking up’ prolonged periods of sitting with light-intensity activities can confer cardio-metabolic health benefits in healthy and overweight/obese populations.
Such evidence is particularly relevant to T2D populations – for whom post-meal glucose and blood pressure reductions (particularly in combination) are primary therapeutic goals. However, whether such benefits extended to those with T2D was unknown.
To examine the relevance for those with T2D, we conducted the REsistance and WAlking breaks in Reducing Diabetes (REWARD) study, which primarily aimed to examine whether frequent brief interruptions to prolonged sitting improved post-meal cardio-metabolic risk markers in adults with T2D.
The main goal of the article is to give you a sound-bite overview of what we did and observed, and the potential implications of the findings.
WHAT DID WE DO?
In a randomized crossover study, 24 sedentary men and women with diet/Metformin treated T2D acted as their own controls and completed 3 x intervention days, with about a week between each day.
The participants were fed standardized meals (similar to a typical Western diet) during the 2-day lead-in period and during each of the intervention days to control for the influence of diet. Basically, all factors that we thought could influence the measures/outcomes of interest were kept the same, while we manipulated the participants’ sitting and activity patterns across each intervention day.
On one intervention day participants sat continuously (SIT) for 7 hours (except for standardized toilet breaks). One the other two intervention days they completed the exact same protocol, but performed regular activity ‘breaks’ for 3 min every 30 min (totalling 36 min) over the 7 hours. These 3 min breaks consisted of either light-walking (LW) on a treadmill at 3.2 km/h or simple body-weight resistance activities (SRAs; half-squats, calf raises, brief gluteal contractions and knee raises).
Figure 1 below gives a basic overview the study intervention days and measures.
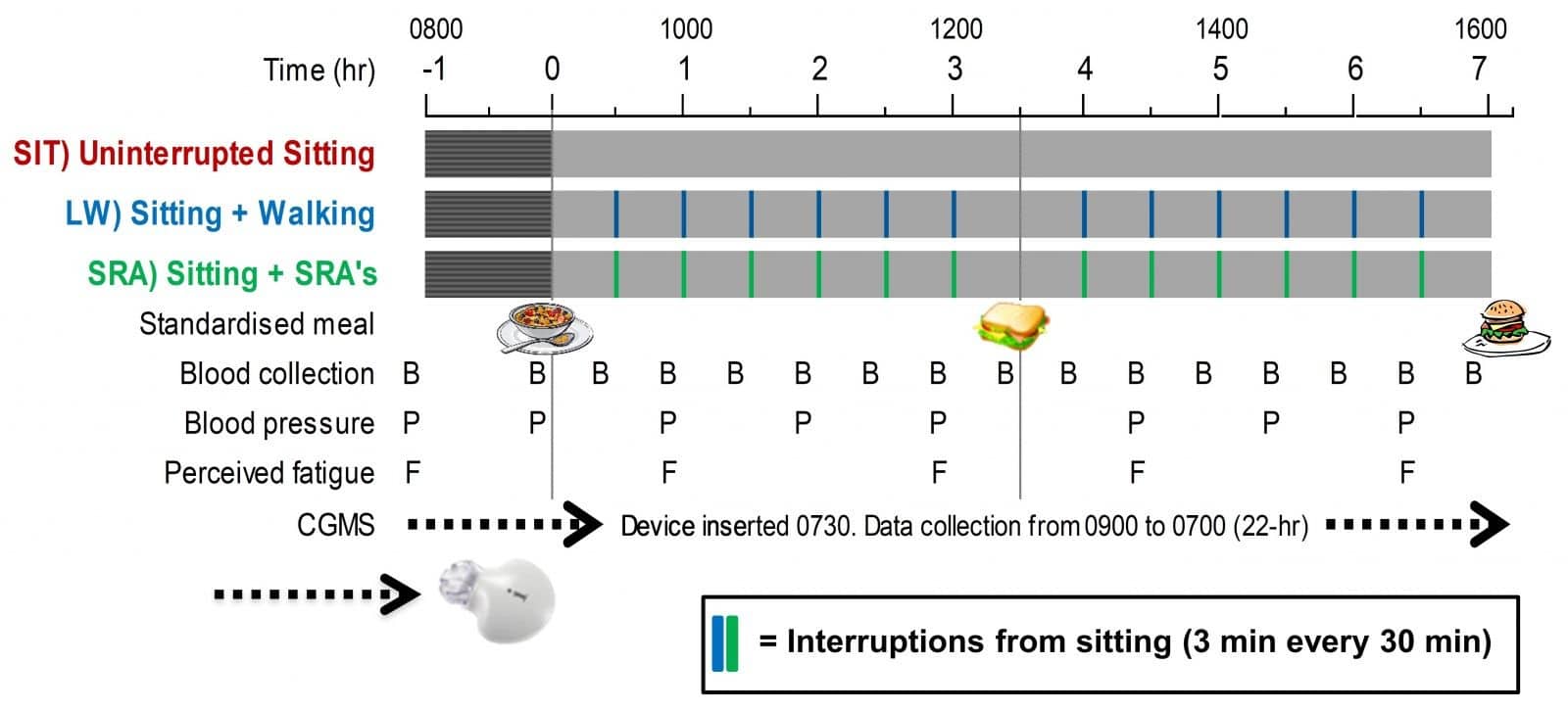
Fig1. Basic overview of the study intervention days/measures.
You may be wondering – why SRAs? There were a few reasons, but the main one was that we felt they may provide a practical alternative to walking (e.g. which usually obliges one to leave the immediate workspace) while also requiring only small amounts of floor space and no specialised equipment. We also thought the different modality of activity ‘break’ would be interesting to test, since resistance exercise is often a somewhat neglected element in physical activity recommendations. Figure 2 provides a basic schematic of what the SRAs looked like, or check out this video – which participants actually mimicked during the trial.
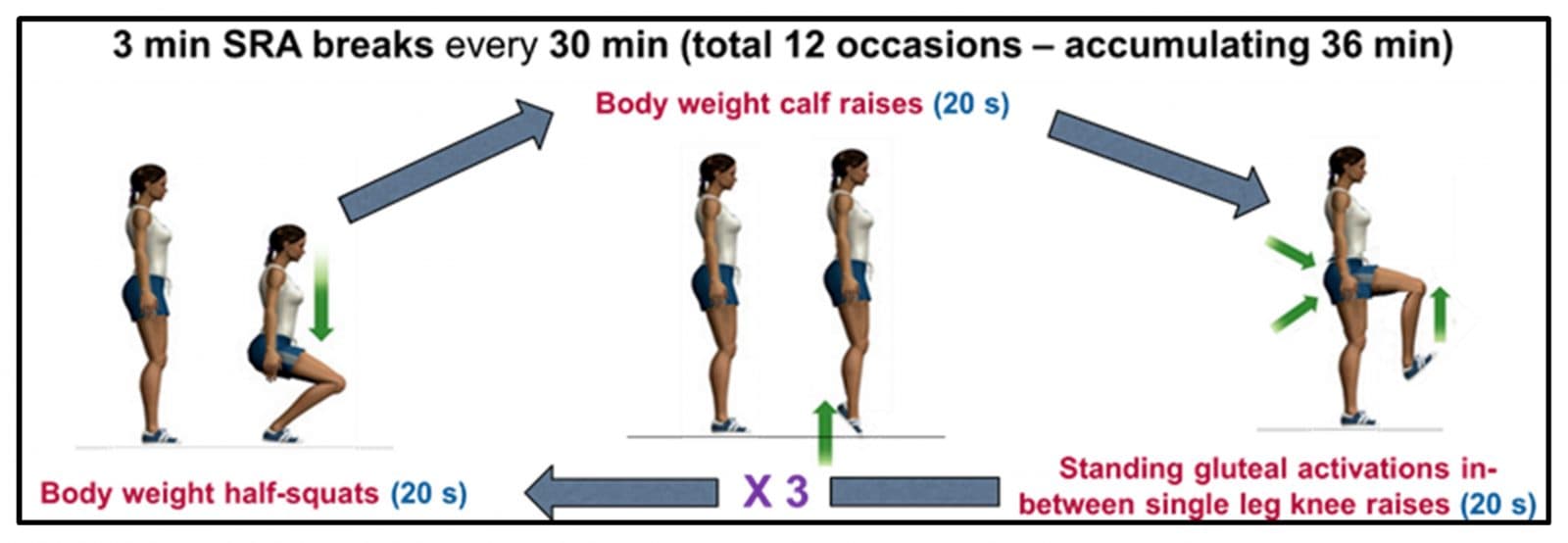
Fig 2. Simple resistance activities (SRA) schematic.
WHAT WE FOUND: BREAKING UP SITTING TIME HAS MULTIPLE BIOLOGICAL BENEFITS FOR THOSE WITH T2D
Parallel cardio-metabolic changes in the laboratory
Compared to the SIT condition, breaking up prolonged sitting with either the LW or SRAs attenuated the detrimental ‘spikes’ in post-meal circulating glucose, insulin and c-peptide blood concentrations (see Figure 3). Post-meal triglyceride (blood fat) concentrations were also lowered for both activity conditions; however, this lowering was only statistically significant for the SRAs. We also saw reductions in resting systolic and diastolic blood pressure levels across the day by ~10-16 mmHg and reductions in plasma norepinephrine concentrations (an indirect marker of sympathetic activity) by 11-18%, with the SRAs resulting in significantly greater lowering than LW for both outcomes.
Looking more deeply into the lipid findings, we saw that both the LW and SRAs were associated with reductions in pro-inflammatory lipids and increases in antioxidant capacity of other lipids compared to SIT, including some differential changes in some lipid species related to platelet activation. This has provided new insights into potential candidate mechanisms (inflammation and oxidative stress) that may help understand why breaking up sitting, particularly in the post-meal state, may be of benefit.
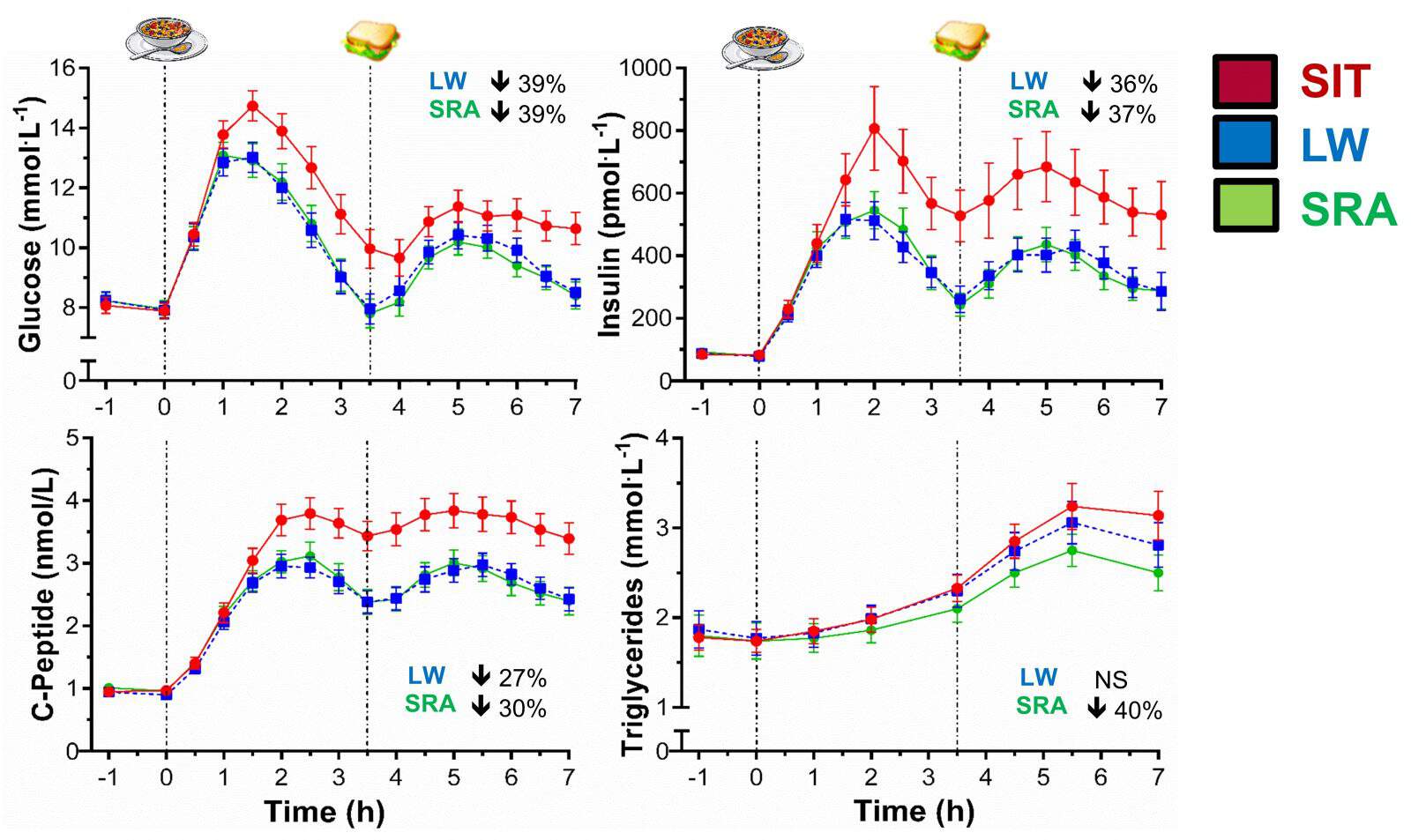
Fig 3. Post-meal (parallel) glucose, insulin, c-peptide and triglyceride responses to thr intervention days.
Nocturnal persistence in glycaemic benefits
Since we also had participants wear continuous glucose monitors (which measure glucose in the interstitial fluid just under the skin every 5 min), we were able to capture glucose concentrations after participants vacated the controlled laboratory setting and returned home to their free-living environments (while still under dietary control). Interestingly, we saw carryover improvements in glycaemic control with the LW and SRA conditions until the next morning (see Figure 4), with an average waking glucose reduction of ~2.7 mmol/L compared to SIT. Notably, participants spent on average 57% and 62-69% less time in overall (22-hour) and nocturnal hyperglycaemia (blood glucose >10 mmol/L), respectively, for both the LW and SRA conditions compared to SIT.
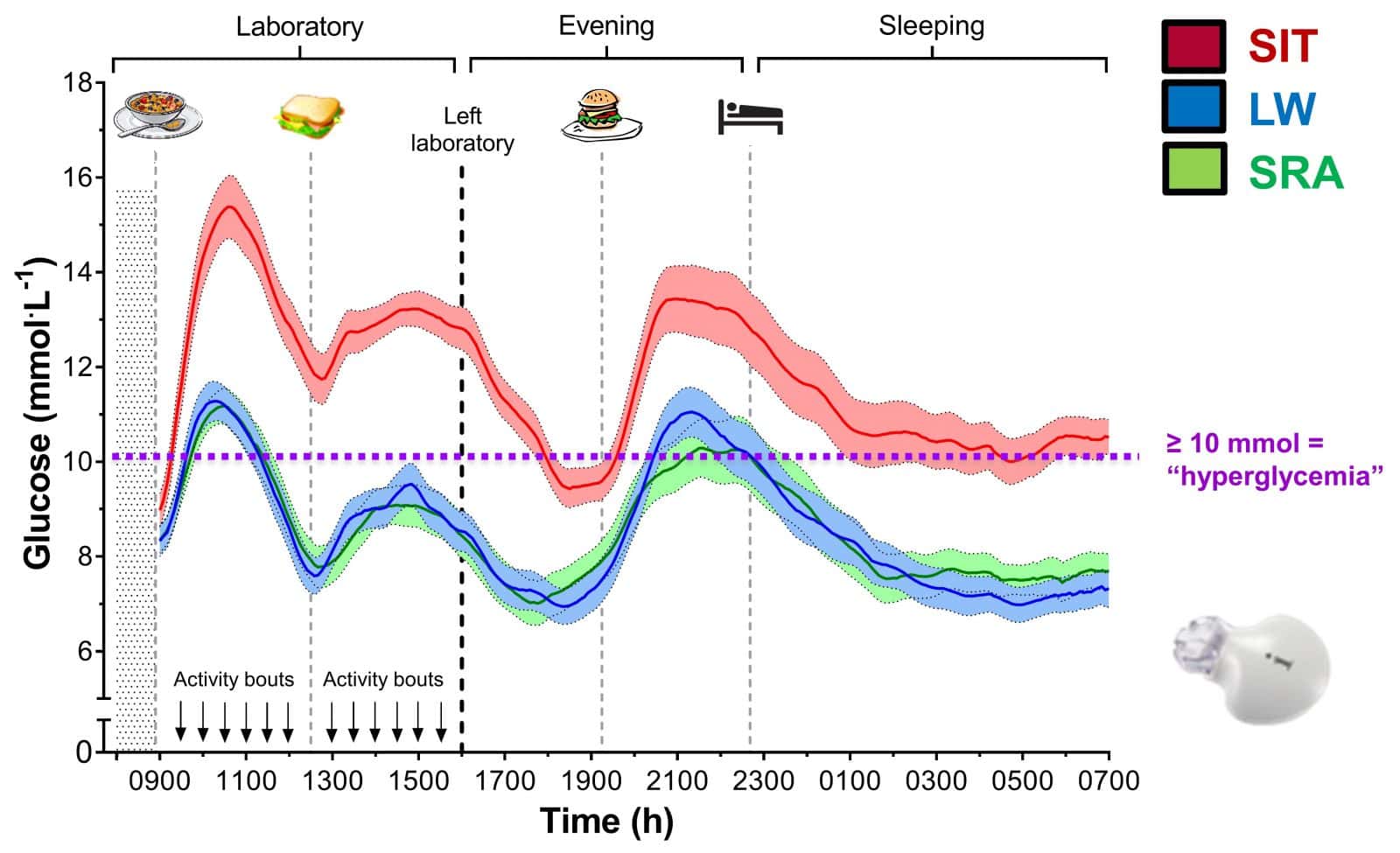
Fig 4. Interstitial glucose concentrations (as measured by continuous glucose monitoring) during the intervention days, showing sustained differences overnight (i.e. carryover effects favouring the breaks conditions after leaving the controlled laboratory setting) while participants slept, until the next morning.
How the participants felt?
For those less excited by the promise of ‘improved cardio-metabolic risk’ dangled as the carrot, we also explored how fatigued and energised participants felt before, during and after the day of prolonged sitting, by implementing visual analogue scales across the trial days.
Participants reported feeling progressively more fatigued (by 29%) across the SIT day, while no meaningful changes in fatigue were apparent on the LW and SRA conditions (see Figure 5). Although we thought the changes in fatigue during the SIT condition may have been related to parallel decrements in glucose control variability, we found no clear evidence to suggest that this was the case. Clearly, things are a bit more complicated…
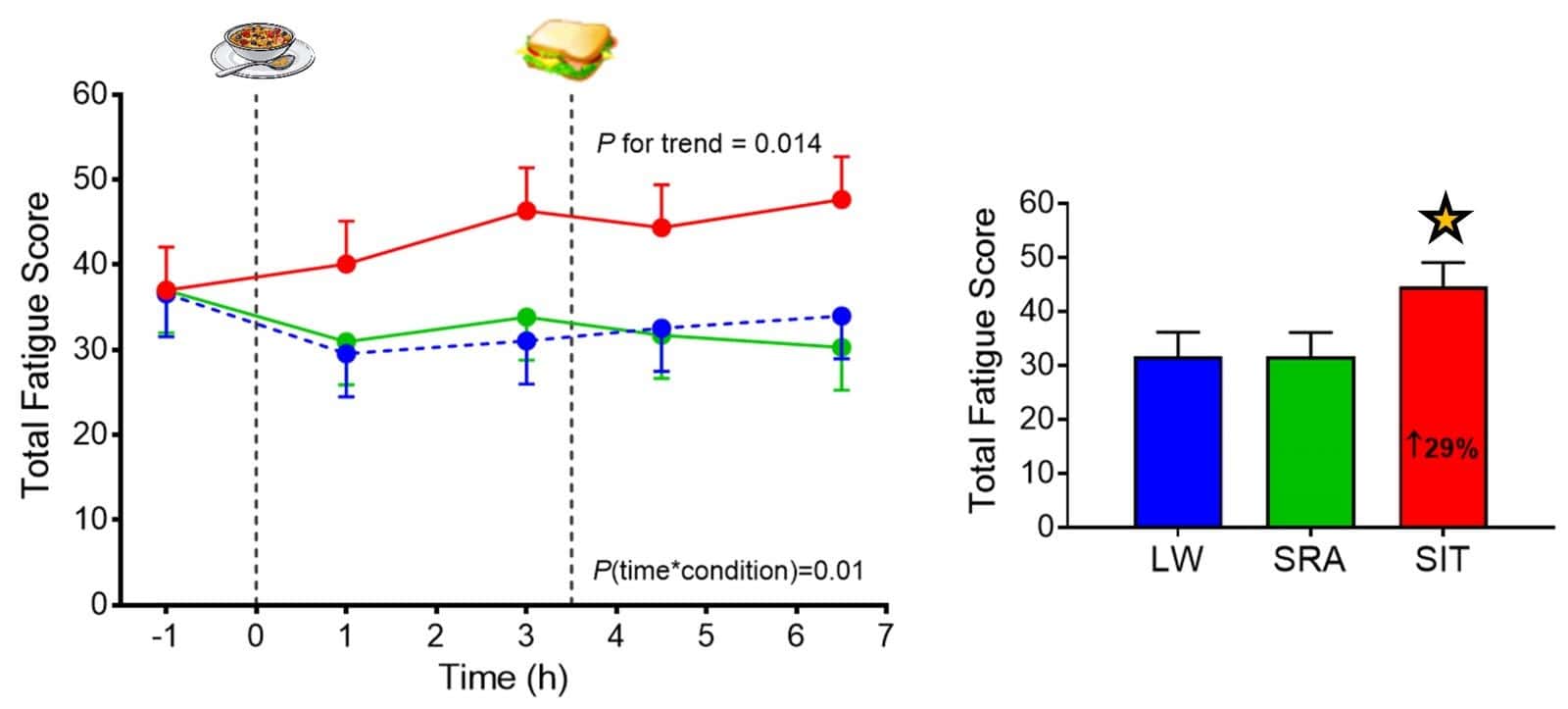
Fig 5. Post-meal (parallel) subjective fatigue responses to the intervention days.
Although preliminary and somewhat limited, we found the fatigue results particularly interesting, as there may be important implications for workplace productivity, self-care regimens (e.g. medications, diet and exercise) and diabetes-related quality of life for those with T2D.
For example, imagine a person with T2D coming home from a long day of sitting in front of a desk and feeling 1) fatigued and sluggish versus 2) more energetic and bubbly. How might scenarios 1 versus 2 impact on the likelihood of this person going outside for an after-work walk or slumping down in front of the television, being pleasant or intolerant with their friends/partner/kids, or subsequently preparing a healthy meal or ordering takeout food? Could prolonged sitting beget other unhealthy behaviours or vice-versa, or, alternatively, could more regular movement precipitate a ‘cascade’ of other healthy behaviours? Although we’ll never know from our particular study, it poses some interesting questions to consider in future research…
WHERE ARE WE AT NOW?
Our initial experimental evidence in T2D patients, along with those of others, has played a role in the American Diabetes Association’s recently updated Position Statement on exercise in diabetes, which now includes recommendations to reduce and interrupt prolonged sitting, as part of a ‘whole-day’ approach to encourage more frequent movement. While these recommendations are stated only in broad terms, given the preliminary evidence, they provide a useful starting point in creating more awareness about the potential impact of total and prolonged sitting exposures. However, as always in science, much still remains to be refined and figured out.
WHAT WE STILL DON’T KNOW, AND WHERE TO NEXT?
We’ve written this review and commentary that discuss the above evidence and its limitations in more depth. We’ve also highlighted the need for more realistic or ‘real-world’ studies in free-living settings in various population groups, the importance of longer-term intervention evidence (weeks-months-years) to justify and inform specific sedentary behaviour recommendations for clinical practice, and public health / environmental policies aiming to maximise cardio-metabolic health benefits.
For example, questions still remain about what durations/thresholds of sitting time are particularly detrimental, in whom, and for what health outcomes, and what mode/duration/intensity of activity that sitting time is best replaced or swapped with. In addition, more in-depth examination of the behavioural feasibility to change, and the relevant mechanisms associated with prolonged sitting, will be important in providing an informed basis for clinical guidelines (i.e. how and why is it important to change, and in whom?).
Future research on the attributes of urban environments and workplaces that promote too much sitting is also warranted, along with innovative, low cost, and sustainable behaviour-change strategies that can reach a large proportion of the population who are at increased risk of cardio-metabolic diseases.
WHAT ARE THE TAKE HOME MESSAGES?
Humans are designed to move. Our biological systems function optimally when we are regularly physically active. The prolonged periods of sitting that now characterise much of our day to day lives – especially our working lives – are missed opportunities for healthy movement. Indeed, the consequences of not taking these opportunities may be particularly pertinent for those with T2D, and sitting less seems unlikely to do harm.
With the ubiquity of sedentary behaviours and the challenges for many of those with T2D of adhering to structured exercise, it seems prudent to advise: ‘Moving More AND Sitting Less’, particularly after meals, as part of a more malleable and comprehensive ‘whole-of-day’ approach. This behavioural strategy may be an acceptable starting point (or ‘gateway’) for the large proportion of T2D patients who are ageing, currently sedentary, overweight/obese, deconditioned, or unable/reluctant to embark upon structured exercise. However, the generalisability, longer-term efficacy and durability of these potential benefits, including a deeper understanding of the mechanisms that may underlie them, should be emphasised in future research.
Importantly, this emerging evidence does not contradict nor downplay the importance of regular participation in moderate-vigorous exercise or improving diet quality, which remain centrepieces of clinical and public health recommendations. Rather, what we are learning about sedentary behaviour is further highlighting and expanding our understanding of the crucial importance of regular movement for T2D prevention and management. There may be individual and population health translational potential through more specific – evidence-based – public health guidelines, programs and policies, including workplace health and productivity initiatives. However, these challenging pieces of the behaviour change and research translation puzzle will need to be addressed and implemented in future research.
About the author: Paddy Dempsey is a Research Fellow at the Baker Heart & Diabetes Institute and Swinburne University in Melbourne, Australia. Paddy has groundings in human physiology, exercise science and public health, and utilises epidemiological, mechanistic/clinical and interventional research methods to enhance research discovery and translation. His research interests are currently focussed on the role of sedentary behaviour, physical activity and diet (including their interacting effects) in the prevention and management of chronic diseases, particularly type 2 diabetes and cardiovascular disease. You can connect or find out more about Paddy on twitter or at his Baker Institute profile page. If you would like personal access to any of the papers cited in this article, you can request copies from Paddy via ResearchGate.