Screen time predicts delays in child development, says new research
February 13, 2019
New Class Announcement: Embodied Anatomy and the Sitting Disease Epidemic
March 11, 2019Today’s article comes from the research team of Professor Stephen Heung-Sang Wong. More about the team can be found at the bottom of this post. This article was originally published in Pediatric Exercise Science entitled “Compliance and practical utility of continuous wearing of activPALTM in adolescents”.
Low compliance rate is often cited as a limitation in studies involving the objective measurement of movement behaviors. This article focuses on the investigation of compliance rate and practical utility of the activPALTM in Hong Kong, a location with a subtropical climate.
The use of the activPALTM
The activPALTM (PAL Technologies Ltd., Glasgow, UK) has been widely applied as an accurate measure of free-living sedentary time and physical activity (1-3). It is generally placed on the participant’s skin at the midpoint of the anterior aspect of the right thigh using a waterproofed transparent film over a week. As such, environmental factors such as climate may inevitably influence compliance with continuous wearing. Practical utility of activPALTM have been assessed in high latitude regions with relatively low annual temperatures such as Glasgow, UK (4-15ºC per year) (4), Waarschoot, Belgium (5-19ºC per year) (5), Maastricht, Netherlands (3-18ºC per year) (6), Nottingham, UK (4-17ºC per year) (7), Bethesda, US (3-27ºC per year) (8), and Brisbane, Australia (15-25ºC per year) (9). Our study examined this issue in Hong Kong, a subtropical climate with an average yearly temperature of 16-29ºC and relative humidity of 70%-89% (10).
Compliance rate with the activPALTM
Most cross-sectional studies in free-living environments using activPALTM have adopted a continuous (24-hour) wear protocol for 7 consecutive days (11). In this way, the accuracy of estimates of PA levels and sedentary time greatly depend on the compliance over the wear period (12). In our study, 755 adolescents (11-18 years; 50.6% girls) wore an activPALTM and 77.9% of them (n=588; 11-18 years; 50.2% girls) provided data that was suitable for analysis. The results showed that 92.6% of participants had ≥ 1 valid day (≤ 240 mins of summed non-wear time in one day), 88.2% had ≥ 2 valid days, 81.6% had ≥ 3 valid days, 76.3% had ≥ 4 valid days, 71.7% had ≥ 5 valid days, 66.6% had ≥ 6 valid days, and 54.9% had ≥ 7 valid days. Overall, 72.4% (426 participants) had at least 3 valid weekdays and 1 valid weekend day in the 7-day period. This compliance rate is lower than those reported in previous studies in adolescents (ranging from 76.7% to 91.9%) (13-16).
What is the practical utility of the activPALTM?
Some practical utility issues including participants’ refusal to comply and device removal are significant sources of reduced compliance in free-living environments (7). In our study, we used a removal log diary and a practical utility questionnaire to investigate this issue. Among the 290 recorded removal episodes, sweat-induced device fell off (25.2%) and skin irritation (39.0%) were the two major reasons. The latter one have also been reported in previous studies for preschool children (38%) (5) and young adults (33.3%) (6).
Our practical utility questionnaire results showed that 45.8% of the participants did not regard the device as having an influence on their activities of daily living, whereas 16% would rather not wear it again. In contrast, a previous study (4) found that 70% of the parents of participants (preschoolers) did not regard the device as interfering with the daily lives of their children and 5% would rather not want their children to wear it again. When defining painful feelings with regards to device wear, application and removal, removal of the device was regarded as painful by nearly half of the participants (46.6%), while the 7-day wearing stage and application stage were regarded less painful. In general, most participants found the activPALTM 24-hour wear protocol acceptable to wear for 7 days. However, compared with other waist-worn or wrist worn devices which can be taken off more easily, it appears that it is more difficult and painful for children and adolescents to remove the activPALTM.
Factors influencing the compliance of the activPALTM
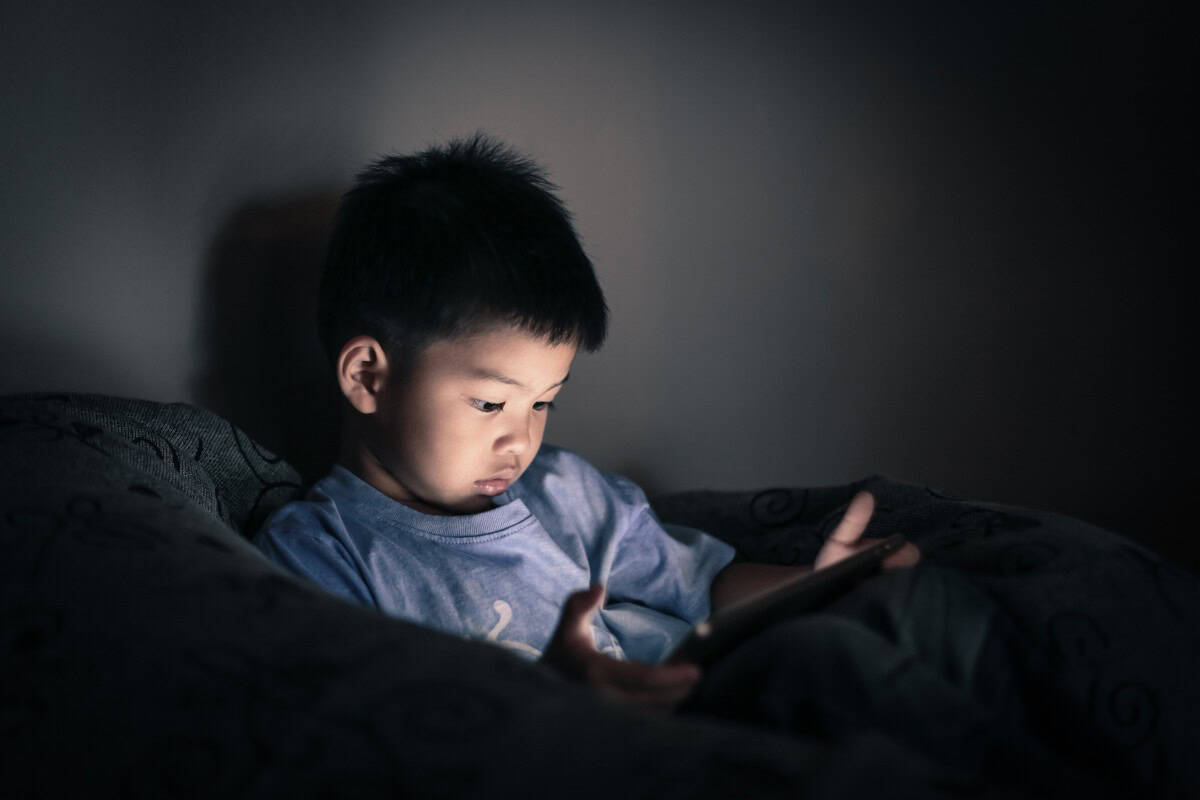
Weather
Four weather parameters were examined in their association with compliance of wearing activPALTM, i.e., temperature, relative humidity, rainfall, and hours of sunlight. Higher compliance rates were found on days of less rainfall among girls. Skin irritation problems such as itchy skin and allergic reactions were more prevalent on rainy days (17), and thus might have resulted in greater device removal and an overall lower compliance. One possible reason why rainfall was negatively associated with wear time in girls and not boys is that in local schools, the uniforms are skirts for girls and trousers for boys. As a result, the activPALTM dressing is more likely to getting wet on rainy days among girls.
Device model and size
Interestingly, the use of the smaller and lighter model (activPALTM micro) did not yield any difference in compliance rates compared to the original model (activPAL3CTM). It is plausible that children of younger age may be more sensitive to the size of the device.
Practical strategies
To improve compliance, our study applied two strategies: (1) using alcohol pads to clean the skin before attachment and (2) placing cartoon stickers on the top cover of the device to increase the visual attractiveness. Compared with the non-use of alcohol pads and cartoon stickers, the use of alcohol and cartoons was associated with 2.8 more valid days in girls and 2.2 more valid days in boys.
What are the suggestions for future users of the activPALTM?
Skin irritation and sweat-induced inadvertent drops were the two major reasons for device removal. We need more user-friendly protocols to enhance the compliance of continuous wearing of the activPALTM. Increasing the visual attractiveness of the device (such as placing cartoon stickers) and enhancing the attachment method (such as using the alcohol pads to clean the skin) are helpful to maximize compliance among children and adolescents.
Furthermore, researchers should consider the environment and the negative influence that precipitation has on protocols for wearing the activPALTM. Providing the participants with additional tapes and sufficient instructions on how to change the adhesive tapes may be helpful in enhancing the compliance.
References
- Kim Y, Barry VW, Kang M. Validation of the ActiGraph GT3X and activPAL accelerometers for the assessment of sedentary behavior. Meas Phys Educ Exerc Sci. 2015;19(3):125-37. doi: 1080/1091367X.2015.1054390
- Grant PM, Ryan CG, Tigbe WW, Granat MH. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med. 2006;40(12):992-7. PubMed doi: 10.1136/bjsm.2006.030262
- Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc. 2011;43(8):1561-7. PubMed doi: 10.1249/MSS.0b013e31820ce174
- Davies G, Reilly J, McGowan A, Dall P, Granat M, Paton J. Validity, practical utility, and reliability of the activPAL in preschool children. Med Sci Sports Exerc. 2012;44(4):761-8. PubMed doi: 10.1249/MSS.0b013e31823b1dc7
- De Decker E, De Craemer M, Santos-Lozano A, Van Cauwenberghe E, De Bourdeaudhuij I, Cardon G. Validity of the ActivPAL™ and the ActiGraph monitors in preschoolers. Med Sci Sports Exerc. 2013;45(10):2002-11. PubMed doi: 10.1249/MSS.0b013e318292c575
- Berendsen BA, Hendriks MR, Meijer K, Plasqui G, Schaper NC, Savelberg HH. Which activity monitor to use? Validity, reproducibility and user friendliness of three activity monitors. BMC Public Health. 2014;14:749. PubMed doi: 10.1186/1471-2458-14-749
- Maddocks M, Byrne A, Johnson CD, Wilson RH, Fearon KC, Wilcock A. Physical activity level as an outcome measure for use in cancer cachexia trials: a feasibility study. Support Care Cancer. 2010;18(12):1539-44. PubMed doi: 10.1007/s00520-009-0776-2
- Steeves JA, Bowles HR, McClain JJ, Dodd KW, Brychta RJ, Wang J, Chen KY. Ability of thigh-worn actigraph and activPAL monitors to classify posture and motion. Med Sci Sports Exerc. 2015;47(5):952-9. PubMed doi: 10.1249/MSS.0000000000000497
- Clark BK, Winkler E, Healy GN, et al. Adults’ past-day recall of sedentary time: reliability, validity and responsiveness. Med Sci Sports Exerc. 2013; 45(6):1198-207. PubMed doi: 10.1249/MSS.0b013e3182837f57
- Hong Kong Observatory. Daily Weather Summary and Radiation Level [Internet]. Hong Kong Observatory, 2000. [Cited 2017 Nov 1]. Available from: http://www.hko.gov.hk/wxinfo/dailywx/dailywx.shtml.
- Edwardson CL, Winkler EA, Bodicoat DH, et al. Considerations when using the activPAL monitor in field-based research with adult populations. J Sport Health Sci. 2017; 6(2):162-178. PubMed doi: 10.1016/j.jshs.2016.02.002
- Matthews CE, Hagströmer M, Pober DM, Bowles HR. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. 2012; 44(1 Suppl 1):S68-S76. PubMed doi: 10.1249/MSS.0b013e3182399e5b
- McCrorie PR, Duncan E, Granat MH, Stansfield BW. Seasonal variation in the distribution of daily stepping in 11-13 year old school children. Int J Exerc Sci. 2015; 8(4):5. PubMed
- Dowd KP, Harrington DM, Bourke AK, Nelson J, Donnelly AE. The measurement of sedentary patterns and behaviors using the activPAL™ Professional physical activity monitor. Physiol Meas. 2012;33(11):1887. PubMed doi: 10.1088/0967-3334/33/11/1887
- Dowd KP, Harrington DM, Hannigan A, Donnelly AE. Light-intensity physical activity is associated with adiposity in adolescent females. Med Sci Sports Exerc. 2014; 46(12):2295-300. PubMed doi: 10.1249/MSS.0000000000000357
- Harrington DM, Dowd KP, Bourke AK, Donnelly AE. Cross-sectional analysis of levels and patterns of objectively measured sedentary time in adolescent females. Int J Behav Nutr Phys Act. 2011;8:120. PubMed doi: 10.1186/1479-5868-8-120
- Meffert JJ. Environmental skin diseases and the impact of common dermatoses on medical readiness. Dermatol Clin. 1999; 17(1):1-17. PubMed
 About the authors: Stephen Heung-Sang Wong (corresponding author) is a Professor and Chairman of the Department of Sports Science and Physical Education, The Chinese University of Hong Kong. His research focuses on physical activity and sedentary behavior for children and youth. You can find out more about Stephen via ResearchGate. Yan Shi (leading author) is a PhD student at the same Department. Her research interest is parental influences on physical activity, sedentary behavior and sleep among youth.
About the authors: Stephen Heung-Sang Wong (corresponding author) is a Professor and Chairman of the Department of Sports Science and Physical Education, The Chinese University of Hong Kong. His research focuses on physical activity and sedentary behavior for children and youth. You can find out more about Stephen via ResearchGate. Yan Shi (leading author) is a PhD student at the same Department. Her research interest is parental influences on physical activity, sedentary behavior and sleep among youth.